Best Practice
Targeted Treatment: Selecting Patients for Renal Denervation
September 22, 2025
Renal denervation (RDN) has emerged as a transformative adjunctive therapy for patients with uncontrolled or resistant hypertension. As clinical evidence and regulatory approvals accumulate, the focus is shifting toward refining patient selection—a critical step to ensure optimal outcomes and avoid unnecessary interventions.
Guideline-Based Criteria: ESC and ESH Recommendations
The 2024 ESC Guidelines and 2023 ESH Guidelines provide a structured framework for identifying suitable RDN candidates:
ESC 2024 Recommendations¹
- RDN may be considered for patients with resistant hypertension (uncontrolled BP despite ≥3 antihypertensive drugs, including a diuretic), if performed in a medium-to-high volume center and following a shared decision-making process.
- RDN may also be considered for patients with uncontrolled hypertension on fewer than three drugs, particularly if they have high cardiovascular risk and express a preference for RDN.
- RDN is not recommended for patients with eGFR <40 mL/min/1.73 m² or secondary hypertension.
ESH 2023 Recommendations²
RDN can be considered in patients with:
- Uncontrolled BP despite combination therapy.
- Drug intolerance or poor quality of life due to side effects.
- Resistant hypertension with eGFR >40 mL/min/1.73 m².
- Emphasis is placed on shared decision-making and treatment in specialized centers.
Insights from Clinical Research³
According to a recent review in Nature Reviews Cardiology, RDN has demonstrated efficacy across the spectrum of hypertension—from mild to truly resistant cases 1. Importantly, the review underscores that higher baseline BP is the most consistent predictor of response. It also highlights the need for:
- Exclusion of secondary hypertension.
- Objective assessment of medication adherence.
- Multidisciplinary evaluation, including hypertension specialists and interventionalists.
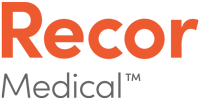
Practical Patient Selection Form
The patient selection form developed by Recor Medical aligns with these guidelines and offers a practical checklist for clinicians. Key inclusion criteria include:
- Office systolic BP ≥140 mmHg despite lifestyle changes and medication.
- Use of at least three antihypertensive drugs, ideally one diuretic.
- No secondary causes of hypertension.
- eGFR ≥40 mL/min/1.73 m².
- Patient willingness to undergo RDN after informed discussion.
Indicators of cardiovascular risk and their guideline relevance
The following factors that may increase cardiovascular risk, listed in the patient selection form, are directly supported by ESC/ESH recommendations1,2:
- Prior Stroke or Transient Ischemic Attack (TIA)
These cerebrovascular events signal advanced vascular disease and are associated with poor outcomes in uncontrolled hypertension. ESC guidelines recognize stroke history as a marker of elevated cardiovascular risk - Prior Myocardial Infarction (MI) and Coronary Artery Disease (CAD)
Patients with a history of MI or CAD are at high risk for recurrent events. ESC guidelines recommend intensive blood pressure control in these populations, and RDN may be considered when pharmacological therapy is insufficient or poorly tolerated - Heart Failure
Hypertension is a major contributor to heart failure progression. ESC guidelines note that patients with heart failure and uncontrolled BP may benefit from RDN, especially when sympathetic overactivity is present - Atrial Fibrillation (AF)
AF is both a consequence and a contributor to hypertension-related cardiac remodeling. ESC documents highlight AF as a comorbidity that increases cardiovascular risk and may support RDN consideration - Smoking
A modifiable risk factor that compounds vascular damage and increases overall cardiovascular risk. While not a direct indication for RDN, smoking status contributes to the global risk profile used in patient selection - Diabetes Mellitus
ESC guidelines provide detailed recommendations for managing hypertension in diabetic patients, emphasizing the need for aggressive BP control. RDN may be considered in those with poor control or medication intolerance. - Peripheral Vascular Disease (PVD)
PVD reflects systemic atherosclerosis and is associated with increased cardiovascular morbidity. ESC guidelines include PVD in the risk stratification for hypertension management
Patients with these conditions were not studied in Recor’s clinical trials, see important information about the device’s indication. Furthermore multidisciplinary evaluation by a team of different medical specialties, and patient-centered treatment decision-making for potential patients who may benefit from catheter-based RDN is encouraged.
References:
| 1 | European Heart Journal, ehae178, https://doi.org/10.1093/eurheartj/ehae178 |
| 2 | Mancia G. et al. J Hypertension 2023 |
| 3 | L. Lauder et all.; Nature Reviews Cardiology volume 22, pages 675–688 (2025) “European guidelines for hypertension in 2024: a comparison of key recommendations for clinical practice”; Expert Recommendation; Published: 21 July 2025 |
December 10, 2025
This article is about the experience of how Dr. Ivan Javier Núñez-Gil built a successful uRDN Program in Spain. It is a powerful example for physicians and institutions looking to innovate and offer patients the latest therapeutic alternatives.
June 26, 2025
In this article, Professor Joachim Weil explores the pivotal role of patient empowerment in the context of renal denervation for treatment-resistant hypertension.
March 11, 2025
For three years, Sergiu's life was dominated by extreme high blood pressure – an invisible yet life-threatening burden.