GUIDELINES
RDN Guidelines
RDN Guidelines
Patient Selection
Controlled hypertension
Controlled hypertension
Controlled hypertension
Uncontrolled hypertension*
Uncontrolled hypertension*
Uncontrolled hypertension*
Resistant hypertension
Intolerant to drugs
Non-adherent to drugs
Non-adherent to drugs
Non-adherent to drugs
High CV risk / severe EOD
1. European Heart Journal, ehae178, https://doi.org/10.1093/eurheartj/ehae178 2. Mancia et al. Journal of Hypertension 2023, 41:1874-2017 3. Zeijen, et al. Neth Heart J (2022) 31, pages3–11 (2023), 4. Kandzari et al. Catheter Cadiovasc Interv. 2021 Sep;98(3):416-426. 5. Rodriguez et al. REC Interv Cardiol. 2022;4:39-46Ï4. 6. Bruno et al. High Blood Press Cardiovasc PrevÏ 2020 Apr;27(2):109-117.
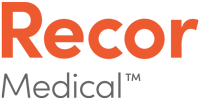
2024 ESC Guidelines on elevated blood pressure
The task force on the management of elevated blood pressure and hypertension of the European Society of Cardiology (ESC) and endorsed by the European Society of Endocrinology (ESE) and the European Stroke Organisation (ESO)
The task force on the management of elevated blood pressure and hypertension of the European Society of Cardiology (ESC) and endorsed by the European Society of Endocrinology (ESE) and the European Stroke Organisation (ESO)
Highlights from the ESC Guidelines¹
- RDN may be considered for patients with uncontrolled resistant hypertension treated with ≥3 anti-hypertensive drugs.
- RDN may be a possible treatment for patients who are non-adherent or intolerant to multiple BP-lowering medications, particularly first-line agents, and who have high predicted CVD risk and a BP that is not at target.
- Patients should express a preference for RDN in a tailored, shared decision-making process.
To reduce BP, and if performed at a medium-to-high volume centre, catheter-based renal denervation may be considered for resistant hypertension patients who have BP that is uncontrolled despite a three BP-lowering drug combination (including a thiazide or thiazide-like diuretic), and who express a preference to undergo renal denervation after a shared risk-benefit discussion and multidisciplinary assessment.
IIb
B
To reduce BP, and if performed at a medium-to-high volume centre, catheter-based renal denervation may be considered for patients with both increased CVD risk and uncontrolled hypertension on fewer than three drugs, if they express a preference to undergo renal denervation after a shared risk-benefit discussion and multidisciplinary assessment.
IIb
A
Due to a lack of adequately powered outcomes trials demonstrating its safety and CVD benefits, renal denervation is not recommended as a first-line BP-lowering intervention for hypertension.
III
C
Renal denervation is not recommended for treating hypertension in patients with moderate-to-severely impaired renal function (eGFR <40 mL/min/1.73 m2) or secondary causes of hypertension, until further evidence becomes available.
III
C
BP, blood pressure; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate. *Class of recommendation. **Level of evidence.
1. European Heart Journal, ehae178, https://doi.org/10.1093/eurheartj/ehae178
Peer-to-Peer Video: ESC Guidelines 2024
Prof Andrew Sharp and Dr Joost Daemen share an overview of the released ESC guidelines for renal denervation (RDN).
ESC Guidelines 2024 – What`s New?
Putting ESC Guidelines into Clinical Practice
ESC Guidelines 2024 – What`s New?
Putting ESC Guidelines into Clinical Practice
2023 ESH Guidelines on Hypertension
The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH)
The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH)
Highlights from the ESH Guidelines¹
- European society has formally recommended RDN (class II)
- Resistant and uncontrolled hypertension
- Uncontrolled HTN despite combination drug therapy or where drugs are poorly tolerated
- Resistant HTN despite the concurrent use of 3 antihypertensive drugs
- Guidelines state the same level of evidence for renal denervation and spironolactone
RDN can be considered as a treatment option in patients and eGFR >40 ml/min/1.73m² who have uncontrolled BP despite the use of antihypertensive drug combination therapy, or, if drug treatment elicits serious side effects and poor quality of life.
II
B
RDN can be considered as an additional treatment option in patients with resistant hypertension if eGFR is >40 ml/min/1.73 m².
II
B
Selection of patients to whom RDN is offered should be done in a shared decision-making process after objective and complete patient’s information.
I
C
*CoR = Class of Recommendation **LoE = Level of Evidence
Mancia G. et al. J Hypertension 2023
2023 SCAI position statement on RDN
Patient Selection Criteria
- Resistant hypertension: BP>130/80 despite 3 meds at maximally tolerated doses
- Uncontrolled hypertension despite lifestyle modification and medication, either intolerant of or do not wish to take additional medications, and willing to undergo RDN after shared decision-making
- Priority to patients with higher CV risk
SCAI Position Statement on Renal Denervation for Hypertension: Patient Selection, Operator Competence, Training and Techniques, and Organizational Recommendations. Swaminathan, R et al. Journal of SCAI, Aug 2023
Institution Qualification
- a primary physician stakeholder with training in the management of HTN and resources for screening, testing, and treating HTN is required.
- an institution interested in performing RDN will require a dedicated HTN program, or ensure appropriate expertise and services of such a program, designed to manage hypertensive patients
- a multidisciplinary team should be identified that shares in the management of potential RDN patients.
2021 RDN Joint Position Statement from SEH-LELHA and the ACI-SEC (Spain)
Objective:
This joint position statement reviews the evidence available on the efficacy and safety profile of renal denervation for the management of hypertension. Based on the results of clinical trials, recommendations have been established on what patients may be eligible for RDN and under what circumstances.
Rodriguez et al. REC Interv Cardiol. 2021.
Summary:
- Possible indications for RDN with data from the latest clinical trials
- Patients with resistant hypertension
- “The SYMPLICITY HTN-3 failed to demonstrate the increased efficacy of RDN vs. sham control. In the recently published RADAINCE-HTN TRIO trial, patients with resistant hypertension treated with a standardized triple combination pill experienced a drop in their BP levels 2 months after RDN compared to a sham procedure.”
- Patients with uncontrolled hypertension
- Patients with frequent hypertensive crises
- Patients with low compliance to pharmacological treatment
- Patients with hypertension-mediated organ damage
- Patients at high cardiovascular risk