Best Practice
Empowered choices: Role of patient involvement in Renal Denervation
June 26, 2025
Prof. Joachim Weil, Heart and Vascular Center, Sana Clinic Lübeck (Germany)
Renal denervation (RDN) has increasingly established itself as a viable therapeutic option for patients with treatment-resistant hypertension. However, a critical question remains: Are we as physicians truly attuned to the preferences and values of our patients?
Over the past several years, it has become clear to me that the success of RDN extends beyond the technical execution of the procedure—it lies equally in recognizing the individual behind the diagnosis. Patients are not passive recipients of medical interventions but should be regarded as active partners in the therapeutic decision-making process.
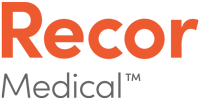
Emerging data from Europe, the United States, and Japan underscore this paradigm shift. A substantial proportion of patients, when appropriately informed, express a preference for RDN over long-term pharmacologic therapy. In some studies, up to 38%1 of patients opted for RDN when presented with the choice, reflecting not only treatment fatigue but also a desire for greater autonomy in managing their condition.
Beyond Blood Pressure: Patient-Centered Communication and Shared Decision-Making in Renal Denervation
The decision to pursue renal denervation (RDN) involves more than clinical criteria—it touches on deeply personal concerns. While physicians focus on blood pressure targets and pharmacologic algorithms, patients are often more preoccupied with side effects, treatment fatigue, and the long-term impact on their quality of life. These are not merely clinical considerations; they are emotional and experiential ones.
Communicating with Clarity and Empathy
To address this disconnect, clear and compassionate communication is essential. I advocate for a style that is accessible, empathetic, and supported by visual analogies. For example, when explaining RDN to patients, I often say: “Imagine your kidney nerves are like a microphone that’s turned up too loud—RDN turns down the volume.” This metaphor allows patients to understand the physiological principle without complex medical terminology. In our clinical practice, we also apply the SOLER technique—Square posture, Open body language, Leaning forward, Eye contact, and Relaxation—to create a setting in which patients feel heard, respected, and actively involved.
Shared Decision-Making: A Clinical Imperative
Shared decision-making is not a rhetorical ideal but a cornerstone of evidence-based, patient-centered care. By presenting all therapeutic options—including RDN, pharmacotherapy, and lifestyle modification—and actively inviting patients to express their preferences, we foster autonomy and ownership of health decisions. This approach has been shown to enhance treatment adherence, improve patient satisfaction, and ultimately lead to better long-term outcomes.
At our center in Lübeck, we have developed a structured follow-up protocol for patients undergoing RDN. This includes regular ambulatory blood pressure monitoring, medication reviews, and individualized lifestyle counseling. Importantly, we integrate patient-reported outcomes to capture subjective experiences and make timely therapeutic adjustments. Preliminary data from our institutional registry demonstrate sustained and clinically significant reductions in both systolic and diastolic blood pressure at 6-month follow-up.
The Future is Personal
Renal denervation is not a one-size-fits-all solution. But when aligned with patient values and expectations, it becomes a powerful tool in our therapeutic arsenal. As physicians, our role is not just to treat—but to listen, guide, and collaborate.
Let’s make patient preference the starting point, not an afterthought.
References:
| 1 | Schmieder R, et al. Clin Res Cardiol. 2019;108:1331-134 |
Disclaimer: The text features Prof. Weil’s medical expertise sharing insights on renal denervation. The views and opinions expressed are those of the doctor and do not necessarily reflect those of Recor Medical or other experts.
December 10, 2025
This article is about the experience of how Dr. Ivan Javier Núñez-Gil built a successful uRDN Program in Spain. It is a powerful example for physicians and institutions looking to innovate and offer patients the latest therapeutic alternatives.
September 22, 2025
Renal denervation is gaining traction as a powerful tool in hypertension management—but it's not for everyone. Discover how ESC and ESH guidelines, clinical evidence, and practical tools like the Recor Medical selection form help identify the right candidates.
March 11, 2025
For three years, Sergiu's life was dominated by extreme high blood pressure – an invisible yet life-threatening burden.